PLEASE NOTE: The January 24-26 course has been canceled due to expected inclement weather.
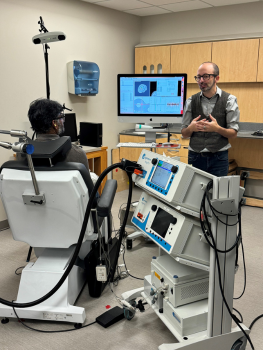
The three-day course offers intensive training on Transcranial Magnetic Stimulation (TMS). TMS is an FDA-cleared treatment for depression, obsessive-compulsive disorder, migraines, smoking cessation and cortical mapping.
Sponsored by the Duke University School of Medicine, the Duke TMS Course includes didactic sessions and hands-on administration of TMS. The didactic sessions with the TMS faculty of Duke University cover all topics relevant to running a TMS clinical service and a TMS research lab, including:
- Device principles and types
- Neuroscience of TMS
- Motor threshold determination
- Treatment technique
- Stimulus dosing
- Risks, complications and contraindications
- Safety screening
- Post-TMS management and continuation treatment
- Clinical and non-clinical research applications
- Emerging brain stimulation techniques
This activity is designed for credentialed clinicians (physicians, nurses, nurse practitioners, and physician assistants) and researchers who wish to enhance their knowledge of TMS and related brain stimulation techniques. The course session is capped at 30 participants.
Duke University Health System Department of Clinical Education and Professional Development designates this live activity for a maximum of 20.0 AMA PRA Category 1 Credit(s). Physicians should claim only credit commensurate with the extent of their participation in the activity.
Please note: Nurses are welcome to take the course and can receive a CME certificate.
Duke University Health System Department of Clinical Education & Professional Development is accredited by the American Nurses Credentialing Center (ANCC), the Accreditation Council for Pharmacy Education (ACPE), and the Accreditation Council for Continuing Medical Education (ACCME), to provide continuing education for the health care team.
To learn more, contact Marisa Spurrell at marisa.spurrell@duke.edu.