Across North Carolina, hundreds of children with critical behavioral health needs are living in noisy, chaotic hospital emergency departments. They’re sleeping, eating, and doing schoolwork in windowless rooms, surrounded by a constant flow of other patients experiencing their own medical crises.
This emergency department (ED) setting doesn’t offer the daily routine and activities that help children thrive, nor does it provide a space for these children to receive much needed longer-term treatment. And unfortunately, some children stay for weeks or even months while awaiting transfer to behavioral health-specific settings to better meet their treatment needs.
The limitations imposed by ED environments—designed to evaluate and treat medical and trauma emergencies—add further stress to the families and care teams working to care for and support children with behavioral health emergencies.
To help address this challenge at Duke, leaders from Duke Children’s Hospital, the Department of Psychiatry & Behavioral Sciences, and the Duke Pediatric Emergency Department created the Duke Pediatric Emergency Department Extension Area. It’s a long name for an innovative environment that gives children with medical or behavioral health conditions a safe and quiet place to receive care while they await appropriate disposition.
Emergency Departments & the Pediatric Mental Health Crisis

In 2020, North Carolina experienced a significant increase in unmet need for pediatric behavioral health care. That year, according to the North Carolina Health Care Association, nearly 90 out of every 1,000 pediatric emergency department visits involved an acute behavioral health need.
“There was a giant spike in pediatric behavioral health cases that began with the COVID pandemic, and it’s continued,” said Emily Greenwald, MD, assistant professor of pediatrics and pediatric emergency medicine medical director. “North Carolina and the rest of the nation have not been able to meet the demands for inpatient or outpatient care options. What we’ve been able to do here at Duke is unique.”
“What we’ve been able to do here at Duke is unique.”
— Emily Greenwald, MD
Duke’s Response to the Crisis
Planning and design of the extension area began in December 2023, and Duke Health saw its first patient in this space on February 1, 2024. Through this initiative, children with behavioral health needs may receive care in this emergency department extension area.
The extension area also provides clinicians a safe, private location to evaluate the children and provide needed services while options for appropriate behavioral health care placements are being explored.
“Creating the extension area was a good move. It’s given children more space, and they’re able to interact with each other,” said Rebecca Taylor, MD, assistant professor and medical director of hospital and emergency pediatric psychiatry for Duke Children’s Hospital. “They have more privacy, and it’s enhanced our ability to help them. It’s made our job a lot easier and much more engaging.”
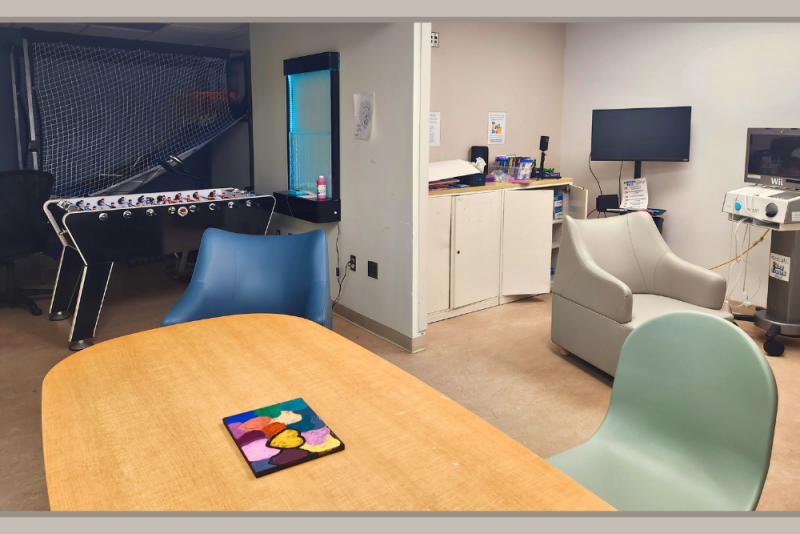
The extension area includes eight private rooms, each with its own bathroom. It also has two open spaces where children can gather to talk or play games; two quiet, sensory-friendly rooms where they can take a break; and safe access to a fenced outdoor courtyard where they can enjoy some fresh air.
According to Sarah O’Rourke, PhD, assistant professor and lead pediatric psychologist for hospital and emergency consultation, the extension area also offers activities to help the children keep a regular schedule.
“We have a very cool collaboration with Child Life [Duke Health’s Child and Adolescent Life team] to bring in fun activities the children didn’t have access to in the medical emergency department,” she noted. Children also have art and music opportunities and access to teachers from Duke’s Hospital School—a collaboration with Durham Public Schools—to help them keep up with their classwork.
Impact of the Extension Area
Since opening its doors in February, the extension area has served nearly 250 patients ranging from 6 to 17 years old. On average, children stay between four and five days; though some patients stay longer, including one patient who stayed for several months.

According to O’Rourke, creating the extension area has led to significant clinical improvement for patients. In the past 10 months, fewer patients have needed a medication intervention or a rapid behavioral response team intervention.
And the positive benefits go beyond the children, Taylor said. It’s also been an uplifting experience for the physicians and nurses on both the emergency medicine team and the psychiatric team.
“The morale among all of us who care for these children has been greatly improved,” she said. “It’s been a great thing, because we all want to be able to continue to do our jobs well and feel like we’re helping these children.”
Ultimately, Taylor noted, the extension area is designed to support young patients waiting for placement, including those with short-term behavioral health needs, while giving them a sense of structure and normalcy.
“It all goes back to protecting their safety, their dignity and their humanity,” she said. “That’s what this extension area is designed to do.”
“It all goes back to protecting their safety, their dignity and their humanity. That’s what this extension area is designed to do.”
— Rebecca Taylor, MD